Obesity is a major health problem. Non Alcoholic Fatty Liver Disease (NAFLD) is the most common cause of chronic liver disease in industrialised countries. According to an epidemiological survey by the Odoxa polling institute, 47.3 % of French adults are obese or overweight (source: http://www.odoxa.fr/sondage/enquete-epidemiologique-nationale-sur-le-surpoids-et- lobesite/).
NAFLD is a global public health burden as it is epidemiologically linked to obesity, type 2 diabetes (T2DM) and metabolic syndrome (SMet).

NAFLD is a global public health burden as it is epidemiologically linked to obesity, type 2 diabetes (T2DM) and metabolic syndrome (SMet).
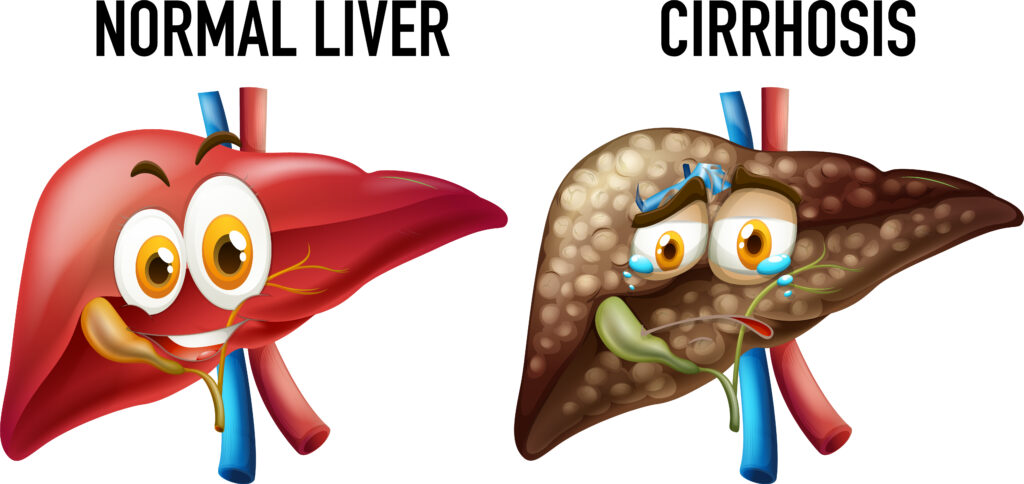
It covers a broad spectrum of liver damage, including simple steatosis, non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis and hepatocellular carcinoma (HCC).
Susceptibility to developing NAFLD varies widely and is influenced by several factors, especially environmental (dietary habits and physical activity) and hereditary (genetic/epigenetic) risk factors. Nevertheless, even the gut microbiota plays a crucial role in the pathophysiology of NAFLD. The interaction between food exposure and the genome is referred to as "nutritional genomics" or "nutrigenetics".
Nutrigenetics will produce new "candidate genes", so called because it is hoped that they are the genes whose alterations cause the phenotype (or disease) under study. In other words, these candidate genes could play a role in predisposing to a diet-related disease, e.g. obesity, cardiovascular disease, osteoporosis, etc.
The aim is to investigate the biological mechanisms involved in acute and sustained genome-nutrient interactions that influence health and may represent a promising field of investigation for improving clinical nutrition and health practice.
The short-term goal is to identify subpopulations that group together genotypes that pose a risk for certain diseases and subsequently refine dietary recommendations. In addition, ethnicity plays a role in dietary intake.

The development of NASH is thought to consist of two successive events. This is the "2-hits" theory proposed by CP Day in 1998 (PMID: 9547102, 1998).
The first event is steatosis, in which there is an excessive accumulation of triglycerides in the cytoplasm of the hepatocytes. This step is accompanied by the appearance of insulin resistance.
In fact, insulin resistance leads to increased lipolysis in adipose tissue and increased gluconeogenesis and triglyceride synthesis in the liver. During my master's studies at the Inserm laboratory in Clamart, we tried to understand the mechanisms of the transition from steatosis to steatohepatitis. We worked with obese, leptin-deficient ob/ob mice and with mice that became obese on a high fat diet (HFD). These mice developed insulin resistance, steatosis and, after injection of lipopolysaccharide (LPS), non-alcoholic steatohepatitis. Through adoptive transfer techniques (transferring cells to another mouse. The cells are usually derived from the immune system to improve the functionality and properties of the immune system). Steatosis has been shown to increase the recruitment of lymphocytes by the liver, and CD4+, T CD8+, and B cells from ob/ob mice, which have the property of specifically migrating to the liver, are greatly increased compared to normal control mice. LPS potentiates this migration. This has shown that the mechanisms of NASH involve not only a liver defect but also an immune defect.
How does it look from a genetic point of view?
NAFLD is considered a complex disease, as interactions between the environment and a susceptible polygenic host determine the phenotype of the disease and influence its progression. In recent years, numerous genome-wide association studies (GWAS, Genome Wide Association Studies) and candidate genes have enriched our understanding of the genetic basis of NAFLD. In particular, variant I148M in the PNPLA3 gene (Patatin-like Phospholipase Domain Protein 3), has been identified as the major common genetic determinant of NAFLD. It was also shown that the identified variants in the TM6SF2 (Transmembrane 6 Superfamily Member 2), MBOAT7 (Membrane Bound O-acyltransferase Domain-containing 7) and GCKR (Glucokinase Regulatory Protein) genes, which have a moderate effect, contribute substantially to the disease. The aim of this analysis is to provide an overview of the state of research on the major genetic and epigenetic modifiers of NAFLD progression. The possibility of translating the increasing wealth of genetic data into the development of new therapies and the clinical translation of diagnostic/prognostic biomarkers will be explored in the future.
NAFLD/NASH and the microbiome?
Research focused on the microbiome offers great opportunities as well as challenges in terms of both pathogenesis and treatment options for NAFLD/NASH. Since most studies to date have applied 16S rRNA sequencing (a classic standard tool for phylogenetic and taxonomic studies of bacteria), which provided low resolution limited to the genus level, it is imperative to identify NAFLD-associated microbes at the strain level using high-precision metagenomic sequencing that also provides functional information about the gut microbiome. Beyond association studies, future research will aim to elucidate the direct causal relationship between gut dysbiosis and NAFLD in animal models and human clinical trials to develop targeted therapies for the microbiota. Despite significant progress in correlating changes in the microbiota with NAFLD, the specific molecular mechanism underlying the interaction between host, environment and microbiome in the development and progression of NAFLD/NASH remains largely unexplored.
In summary, a precision medicine approach based on person, dietary and microbiome profiles could facilitate risk stratification and predict variable clinical phenotypes, diagnostic accuracy and therapeutic response in NAFLD. The incorporation of gut microbiome-based precision medicine, including personalised probiotics (Suez et al, 2018; Zmora et al, 2018) and postbiotic interventions (inanimate microorganisms that are complementary and synergistic to prebiotics, microbiota strains) (Thaiss et al, 2016), may also be an important consideration for the treatment of NAFLD.
Overall, the opportunities and challenges of microbiome research open a new window for future studies that will hopefully elucidate the more specific role of the gut microbiome in NAFLD and establish personalised microbiota-targeted therapeutic approaches.
What about food supplements?
Is there a way to prevent it?
High quality labs offer a combination of supplements that affect the digestion, liver and intestines.
A combination of milk thistle, schisandra, dandelion and antioxidants not only supports liver and bile function, but also detoxifies the body and has antioxidant protection.
You can combine these ingredients with a probiotic that not only provides microencapsulated lactic acid bacteria, but also helps to care for the mucous membranes thanks to vitamins A, B2, B3 and B8. It will help protect cells from oxidative stress, thanks to vitamins B2, C and E, as well as the trace elements zinc, manganese, copper and selenium.
Conclusion
From a global perspective, the genetic and even the epigenetic profile (through sequencing, whether high-throughput or through the various techniques used for epigenetic sequencing), the gut microbiota profile and the ethnicity of the person can influence dietary choices by going beyond the guidelines for a healthy diet at the population level.
However, it is possible to prevent NAFLD and NASH through a healthy lifestyle. Despite the stress we experience every day, it is possible to work on our lifestyle, not only through nutritional supplements, but also through psychotherapeutic support, which can also raise awareness of e.g. food addictions such as sugar, junk food, baking etc.
Yours sincerely.
Dr. (PhD) Joyce EL HOKAYEM
Geneticist and molecular biologist
Naturopathic counsellor and Gestalt therapy therapist.
https://therapeut-naturheilpraxis.de/

